Skin condition
The skin on your feet is exposed to constant pressure, moisture, and friction making it more prone to problems than other areas of the body. This page will guide you through the most common foot skin issues, what symptoms to look out for, and provide some advice on how to self-care.
Corns and calluses
Corns and calluses
Corns and calluses are hard or thick areas of skin that can be painful. They’re not often serious. There are things you can try to ease them yourself.
Symptoms of corns and calluses
You mostly get corns and calluses on your feet, toes and hands.
 Corns are small lumps of hard skin.
Corns are small lumps of hard skin.
 Calluses are larger patches of rough, thick skin.
Calluses are larger patches of rough, thick skin.
 Corns and calluses can also be tender or painful.
Corns and calluses can also be tender or painful.
What you can do about corns and calluses
If you have diabetes, heart disease or problems with your circulation, do not try to treat corns and calluses yourself. These conditions can make foot problems more serious. See a GP or foot specialist.
Corns and calluses are not often serious. There are some things you can try to get rid of them yourself and stop them coming back.
Do
- Wear thick, cushioned socks
- Wear wide, comfortable shoes with a low heel and soft sole that do not rub
- Use soft insoles or heel pads in your shoes
- Soak corns and calluses in warm water to soften them
- Regularly use a pumice stone or foot file to remove hard skin
Don’t
- do not try to cut off corns or calluses yourself
- do not walk long distances or stand for long periods
- do not wear high heels or tight pointy shoes
- do not go barefoot
A pharmacist can help with corns and calluses.
You can ask a pharmacist about:
- heel pads and insoles
- products to treat corns and calluses
- different types of pain relief
See a GP if:
You think you have a corn or callus and:
- you have diabetes
- you have heart disease or problems with your circulation
- it bleeds, or has any pus or discharge
- it has not improved after treating it at home for 3 weeks
- the pain is severe or stopping you doing your normal activities
What we mean by severe pain
Severe pain:
- always there and so bad it’s hard to think or talk
- you cannot sleep
- it’s very hard to move, get out of bed, go to the bathroom, wash or dress
Moderate pain:
- always there
- makes it hard to concentrate or sleep
- you can manage to get up, wash or dress
Mild pain:
- comes and goes
- is annoying but does not stop you doing daily activities
Treatment for corns and calluses
A GP can check if you have a corn or callus.
They might:
- give you antibiotics if a corn or callus is infected
- refer you to a foot specialist if they think you need further treatment
Treatment from a foot specialist
A foot specialist, such as a podiatrist, may be able to offer treatments such as:
- cutting away the corn or callus
- patches to help soften the hard skin so it can be removed
- specially made soft pads or insoles to take pressure off the painful area of your foot
Referral to a podiatrist on the NHS may not be available to everyone and waiting times can be long. You can pay to see a podiatrist privately.
Common causes of corns or calluses
Corns and calluses are caused by pressure or rubbing of the skin on the hands or feet.
For example, from:
- wearing high heels, uncomfortable shoes or shoes that are the wrong size
- not wearing socks with shoes
- lifting heavy weights
- playing a musical instrument
Blisters
Blisters
Blisters often heal on their own within a week. They can be painful while they heal, but you will not usually need to see a GP.
How you can treat a blister yourself
There are things you can do to protect a blister and help stop it getting infected.
Do
- keep the blister as clean as possible, gently wash the skin and pat it dry
- cover blisters with a soft plaster or padded dressing
- wash your hands before touching a burst blister
- allow the fluid in a burst blister to drain before covering it with a plaster or dressing
Don’t
- do not burst a blister yourself
- do not peel the skin off a burst blister
- do not pick at the edges of the remaining skin
- do not wear the shoes or use the equipment that caused your blister until it heals
A pharmacist can help with blisters
To protect your blister from becoming infected, a pharmacist can recommend a plaster or dressing to cover it while it heals. A hydrocolloid dressing (a moist dressing) can protect the blister, help reduce pain and speed up healing.
Symptoms of a blister
 Blisters are small pockets of clear fluid under a layer of skin.
Blisters are small pockets of clear fluid under a layer of skin.
 Blood blisters may look red or black and are filled with blood instead of clear fluid.
Blood blisters may look red or black and are filled with blood instead of clear fluid.
 An infected blister can be hot and filled with green or yellow pus. The surrounding skin may look red, but this can be hard to see on brown or black skin.
An infected blister can be hot and filled with green or yellow pus. The surrounding skin may look red, but this can be hard to see on brown or black skin.
Do not ignore an infected blister. Without treatment it could lead to a skin or blood infection.
Treatment for blisters from a GP
A GP might burst a large or painful blister using a sterilised needle. If your blister is infected, they may prescribe antibiotics. They can also offer treatment and advice if blisters are caused by a medical condition.
Conditions that can cause blisters include:
- Chickenpox: A childhood illness that causes itchy spots
- Cold sores: Small blisters that develop on the lips or around the mouth, caused by a virus
- Genital herpes: A sexually transmitted infection (STI) that most commonly affects the genitals
- Bullous impetigo: A bacterial skin infection
- Pompholyx: A type of eczema
- Scabies: A skin condition caused by tiny mites
- Hand, foot and mouth disease: A viral infection that usually affects young children
How to prevent blisters
Blisters develop to protect damaged skin and help it heal. They’re mostly caused by friction, burns and skin reactions, such as an allergic reaction.
Blood blisters appear when blood vessels in the skin have also been damaged.
If you often get friction blisters on your feet or hands:
- wear comfortable, well-fitting shoes
- wear new shoes for short periods of time, until they’re comfortable
- wear thick socks during exercise, such as moisture-wicking sports socks
- change your socks frequently if you get sweaty feet
- wear protective gloves when you exercise or if you use tools at work
Chilblains
Chilblains
What are chilblains?
Chilblains are small areas of inflamed and often, itchy, skin which develop on fingers and toes. They generally affect the young and old and are caused when blood vessels don’t react normally to cold, damp weather.
Chilblains can be uncomfortable and can become infected if the inflamed skins tears. If people with chilblains protect their fingers and toes from the cold, they will heal within a few weeks.
Look after yourself
- Family history: Chilblains are often a family trait
- Poor circulation or general health.
- Work-related: People working in cold and damp conditions.
- Smoking: Nicotine narrows blood vessels.
- Damaged feet: Chilblains can appear on a bunion or a toe that’s squeezed by tight shoes.
Prevent
- Warm your cold feet up slowly, don’t put your feet in hot water, near direct heat from fires or radiators or use very hot water bottles and wheat bags.
- Improve your circulation through gentle exercise and massage
- Use thermal insoles in shoes and boots
- Stop smoking: Nicotine narrows your blood vessels
- Wear warm clothes and protect your hands, feet and legs from the cold.
- Warm your hands before you go out by soaking them in warm (not hot) water for several minutes and then drying them thoroughly. Wear cotton-lined waterproof gloves if necessary.
- If you have diabetes, regularly check your feet or ask some-one to do this. You may not be able to feel your feet and could have infected chilblains without noticing it.
When to seek professional advice
You should seek medical advice if you think your chilblain may have become infected. Signs of infection may include swelling or pus forming in the affected area, swollen glands, feeling generally unwell and a high temperature of 38C or above.
Further information visit the Royal College of Podiatry
Warts and verrucas
Warts and verrucas
Warts and verrucas are small lumps on the skin that most people have at some point in their life. They usually go away on their own but may take months or even years.
Symptoms of a wart or verruca
 Warts feel firm and rough. They can appear on palms, knuckles, knees and fingers.
Warts feel firm and rough. They can appear on palms, knuckles, knees and fingers.
 Warts are usually skin coloured but may appear darker on black or brown skin.
Warts are usually skin coloured but may appear darker on black or brown skin.

You can get verrucas on your feet. They have tiny black dots under the hard skin.

Some warts are round, flat and can be yellow (plane warts). You can have many of them.

Clusters of warts spread over an area of skin (mosaic warts) are common on feet and hands.
Warts are not harmful, but some people find them itchy, painful or embarrassing. Verrucas are more likely to be painful, like standing on a needle.
You can treat warts if they bother you, keep coming back or are painful.
A pharmacist can help with warts and verrucas
You can buy creams, plasters and sprays from pharmacies to treat warts and verrucas.
These treatments can take up to 3 months to complete, may irritate your skin and do not always work. You should not use these treatments on your face.
Your pharmacist can give you advice about the best treatment for you.
See a GP if
- you’re worried about a growth on your skin
- you have a wart or verruca that keeps coming back
- you have a very large or painful wart or verruca
- you have a wart that bleeds or changes in how it looks
- you have a wart on your face or genitals
Treatments for warts and verrucas
A GP may be able to freeze a wart or verruca so it falls off a few weeks later. Sometimes it takes a few sessions.
Check with the GP if the NHS pays for this treatment in your area.
If treatment has not worked or you have a wart on your face, the GP might refer you to a skin specialist (dermatologist).
If you have a large or very painful verruca, you may be referred to a foot specialist (podiatrist).
A podiatrist can provide a number of treatments including:
- stronger medicines than you can get from a pharmacist
- freezing the verruca using liquid nitrogen (cryotherapy)
- surgery to remove the verruca using a scalpel or laser
You can also pay to see a podiatrist privately.
How to stop warts and verrucas spreading
Warts and verrucas are caused by a virus. They can be spread to other people from contaminated surfaces or through close skin contact.
You’re more likely to spread a wart or verruca if your skin is wet or damaged.
It can take months for a wart or verruca to appear after contact with the virus.
There are things you can do to help stop warts or verrucas spreading to other people.
Do
- wash your hands after touching a wart or verruca
- change your socks daily if you have a verruca
- cover warts and verrucas with a plaster when swimming
- take care not to cut a wart when shaving
Don’t
- do not share towels, flannels, socks or shoes if you have a wart or verruca
- do not bite your nails or suck fingers with warts on
- do not walk barefoot in public places if you have a verruca
- do not scratch or pick a wart
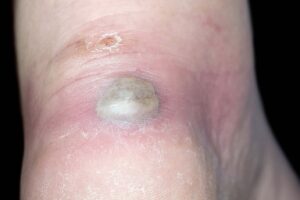
Foot ulcers and wounds
Foot ulcers and wounds
What is a foot ulcer?
An ulcer is a wound that is not healing as expected. Wounds and ulcers can be painful and sometimes ooze clear fluid or pus.
What is a wound?
A wound is any break in the skin.
Common causes
There are many causes (risk factors) such as:
- poor footwear
- complications of diabetes
- loss of fatty padding on the feet
- loss of feeling (neuropathy)
- poor circulation (peripheral arterial disease)
What you can do for yourself
- Eat a well-balanced diet, including protein and a variety of fruit and vegetables.
- Maintain good blood glucose control if you have diabetes.
- If you smoke, try to reduce the number you smoke or consider giving up.
- If you drink alcohol regularly, try to reduce your intake.
When to get professional advice
If you experience any of the following contact your podiatrist, doctor or nurse immediately:
- An ulcer or wound to the foot
- Any new pain or throbbing
- More swelling in the affected area
- Colour changes surrounding the ulcer, for example, redness or blackness
- More discharge or smell from the ulcer
- An increase of heat and warmth in the affected area
- Generally feeling unwell with a raised temperature (38C or above) or nausea.
Treatment
If you need regular treatment to help your foot ulcer to heal we will work out a plan with you which might include some or all of the things listed here:
- Removing dead skin- ulcers sometimes hide under hard skin and can gather dead tissue around them, so dead skin needs to be removed regularly. This might cause slight bleeding which is completely normal.
- Antimicrobial and protective dressings, these might change during your treatment.
- Regular change of dressings: The podiatrist will show you how to change your dressing if you’re able to do this yourself. We’ll make other arrangements if you can’t do this yourself
- Referral to other NHS specialists.
- Wearing special boots or sandals if you can’t wear your own shoes. Some patients may be referred to an orthotist for specialist footwear.
Further information visit the Royal College of Podiatry
Athlete's foot
Athlete's foot
Athlete’s foot is a common fungal infection that affects the feet. You can usually treat it with creams, sprays or powders from a pharmacy, but it can keep coming back.
Symptoms of athlete’s foot

One of the main symptoms of athlete’s foot is itchy white patches between your toes.


It can also cause sore and flaky patches on your feet. The skin can look red, but this may be less noticeable on brown or black skin.


Sometimes the skin on your feet may become cracked or bleed.
Other symptoms
Athlete’s foot can also affect your soles or sides of your feet. It sometimes causes fluid-filled blisters.
If it’s not treated, the infection can spread to your toenails and cause a fungal nail infection.
A pharmacist can help with athlete’s foot
Athlete’s foot is unlikely to get better on its own, but you can buy antifungal medicines for it from a pharmacy. They usually take a few weeks to work.
Athlete’s foot treatments are available as:
- creams
- sprays
- powders
They’re not all suitable for everyone, for example, some are only for adults. Always check the packet or ask a pharmacist.
You might need to try a few treatments to find one that works best for you.
Things you can do if you have athlete’s foot
You can keep using some pharmacy treatments to stop athlete’s foot coming back. It’s also important to keep your feet clean and dry. You do not need to stay off work or school.
Do
- dry your feet after washing them, particularly between your toes, dab them dry rather than rubbing them
- use a separate towel for your feet and wash it regularly
- wear clean socks every day, cotton socks are best
Don’t
- do not scratch affected skin, this can spread it to other parts of your body
- do not walk around barefoot, wear flip-flops in places like changing rooms and showers
- do not share towels, socks or shoes with other people
- do not wear the same pair of shoes for more than 2 to 3 days in a row
- do not wear shoes that make your feet hot and sweaty
See a GP if
You have athlete’s foot and:
- treatments from a pharmacy do not work
- you’re in a lot of pain
- your foot or leg is hot, painful and red (the redness may be less noticeable on brown or black skin), this could be a more serious infection
- the infection spreads to other parts of your body such as your hands
- you have diabetes, foot problems can be more serious if you have diabetes
- you have a weakened immune system, for example, you have had an organ transplant or are having chemotherapy
Treatment for athlete’s foot from a GP
If you have athlete’s foot and treatments from a pharmacy have not worked, a GP may:
- send a small scraping of skin from your feet to a laboratory to check you have athlete’s foot
- prescribe a steroid cream to use alongside antifungal cream
- prescribe antifungal tablets, you might need to take these for several weeks
- refer you to a skin specialist (dermatologist) for more tests and treatment if needed
How you get athlete’s foot
You can catch athlete’s foot from other people with the infection.
You can get it by:
- walking barefoot in places where someone else has athlete’s foot especially changing rooms and showers
- touching the affected skin of someone with athlete’s foot
You’re more likely to get it if you have wet or sweaty feet, or if the skin on your feet is damaged.